Saving a life is a preeminent principle of Jewish ethics, but there are circumstances in which other Jewish values may lead us to make ending a life the priority.
Jewish bioethics has preserving life as a central preoccupation. Early in their studies, rabbinical students learn that piku’akh nefesh dokheh et hashabbat, that saving a life takes precedence even over observing Shabbat.[fn](B. Talmud, Yoma 85a)[/fn] Medicine was at a very early stage of development when saving a life became an uncontested demand in Jewish tradition. At that time, there was little that could be done in the face of a broad array of health crises, and many people died young. Of course, even then some people reached a frail old age. Nevertheless, in a world without antibiotics, cancer treatments, feeding tubes and CPR, to name but a few, there was no reason to raise questions about people living longer than they wished. Living until 120 was a fanciful ideal; most didn’t make it half that far. With the level of medical sophistication that we now have, one criterion for judging bioethical positions is to ask whether they adequately respond to the cases of pain and vulnerability that occur under these changed conditions.
A well-known rabbinic story—one also known in other traditions—concerns a boy whose grandfather has become increasingly messy in his old age. The boy’s father has given the grandfather a wooden bowl to eat from and has instructed him not to sit at the dining table any longer. One day the father sees the boy carving a piece of wood. When his father asks what he is doing, the boy says he is preparing for his father’s old age, just as his father has done for his grandfather. The father immediately invites the grandfather back to the table. The grandfather in the story was feeble but clearly still able to feed himself. The point of the story is our obligation to preserve the kavod, dignity, of those who are declining in physical or mental capacity. While that obligation is particularly strong regarding parents in Jewish tradition, it pertains to others as well.
Loss of Kavod (Dignity)
Someone came to me recently and asked for advice about his wife. She is paralyzed with ALS and experiences her situation as not only a loss of movement but also a loss of kavod, dignity, as she can no longer toilet herself or even wash. She is ready to die, but her family does not believe that they have the right to help her die. So she suffers, and they suffer with her, every day. The gift of briyut, of health, is no longer hers. One way of dealing with this is to stop all her medications, but her doctors have warned that this will be a painful way to die.
One use of a traditional argument is to say that without medical treatment, someone with ALS could be designated a goses (someone within days of death) or t’reyfa (someone with an illness that makes death certain)[fn]See Elliot Dorff, Matters of Life and Death (JPS, 1998), pages 199-200.[/fn], allowing a shift away from preserving life. I laud efforts in that direction for those seeking a halakhic justification for a cessation of the focus on prolonging life. But it seems clear that these terms were not coined for such situations. For those of us who consider ourselves post-halakhic, it seems more comfortable to say that an individual ought to have the right to decide that the value of kavod, dignity, can under some circumstances take precedence over piku’akh nefesh (saving a life). Arguing that requires me to see saving a life as a high value, rather than as an inviolable principle. The halakhah recognized that fact by stating that one could not save one’s own life if it required public idolatry or rape, for example, so balancing values even when a life is at stake is well known within our tradition.[fn]B. Talmud, Sanhedrin 74a-b.[/fn]
By that argument, the woman with ALS has a right to refuse to eat and at a later stage to refuse insertion of a feeding tube. She is making decisions that are l’tovata, in her best interest as she understands it. If she had access to a fatal dose of medicine and took it just before she became too disabled to do it, who could blame her? Certainly not I. If she consented through blinking her eyes and her husband or child administered the fatal dose, I would laud their love and courage.
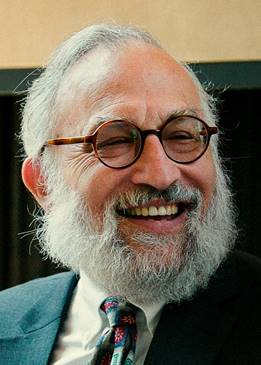
There has been a subtle change regarding suicide in the American Jewish community. When I visited the cemetery in my parents’ hometown of Augsburg, Germany, there was a whole row of graves against one wall of the cemetery. They were all from 1942, when many Jews committed suicide to avoid the dehumanization and suffering of deportation to the concentration camps. The liberal Jewish cemetery nonetheless followed halakhah and buried these suicides along the outer wall of the cemetery. In the United States in recent years, I have not heard of a single suicide buried at the edge of any non-Orthodox cemetery. I am not saying that it does not happen; over the last 75 years, however, it has gone from being standard procedure to a relative rarity.
How can we account for that change? In part, it is a response to our greater understanding of mental illness. In part, it is an acceptance of greater individual autonomy. In part. it represents a desire to be kind to the surviving family. But I believe that it also flows from a growing awareness that there is such a thing as living too long. For some people, their last years are characterized by pain, misery and a sense of indignity, of being imprisoned by their failing minds and bodies. When quality of life ceases forever to exceed the burden and pain of living for an individual, I would argue that it is a rational and Jewishly defensible decision to end one’s life. The pattern in cemeteries offers implicit support for that position. The shift in burial of Jews who have committed suicide is a statement about how Jewish people now views suicide. The beliefs and practices of ordinary Jews ought to be taken into consideration by poskim (halakhic decisors) and Jewish bioethicists in formulating positions on suicide and assisted suicide. I celebrated my aunt’s 90th birthday a few years ago and toasted her with the words bis a hundert und tzwantzig, until 120. She shuddered and responded, “God forbid!”
My mother died when she was 96. In her last years, I spoke with her almost every day. In her eighties, she first gave up tennis, then gave up golf. Her daily walks got shorter and shorter until they stopped altogether. She was too deaf to enjoy movies, music, television or even conversation. More important, over her last years, her dementia got steadily worse. She was forced to give up her beloved bridge games. This once intelligent woman was acutely aware that her competence was draining away. She knew her memory was largely gone. She could no longer remember her grandchildren and great-grandchildren, and she was aware that she could no longer think straight. She could not remember where she put her dentures and without the aides who put away her hearing aids nightly, she would have lost those as well. Her arthritis was an ongoing source of physical pain. She had to relocate to a dementia unit in her continuing-care community.
My brother and I ensured that she received excellent care, and we both remained in regular touch. But neither of us could do much as my mother’s mind slipped away. Should she not have had the right to die in a painless way if that were her choice? She had outlived her friends, her husband, her sister. She could not travel, and she had no activities left in which she takes pleasure. She experienced her growing incompetence as an intolerable burden. Was it not cruel to insist that she ought to live on and on?
In nearly every conversation, she would tell me that she was thinking about suicide. Why did she not do it? She was frightened of the pain she imagined would be involved. And she worried about the social disapprobation. If she could have taken a pill and been certain she would die in her sleep, she would have probably escaped her misery a year or two sooner. If she had known the pill were available, signaling social acceptability for such a decision, she would have found comfort in that even if she had chosen not to take it.
One traditional idea about our role in this world is that our lives are on loan from God, and that we therefore have an obligation to protect them. On the more literal level, this requires a quite traditional God-idea, one which is not consonant with Reconstructionist views of God or with process theology more generally. On a metaphorical level, this is a reference to the obligation to attempt to discern and act upon our holy purpose in this world. If my mother were capable of formulating the thought, she would say that she has no further purpose in this world. She would have a point, because her life is nothing but a burden to her. She does not believe in olam haba (life after death) and therefore has no sense that her current suffering will serve her in good stead in the world to come.
In 2013, euthanasia accounted for 4.6 percent of all deaths in Belgium. The reason given for 7 percent of euthanasia deaths in the Netherlands was that people were “tired of living.” In Oregon, on the other hand, the number of assisted suicides remains very low. We know from the use of assisted suicide in Belgium and the Netherlands that it needs careful regulation. Of course, this requires appropriate legislation guaranteeing that all efforts to move people towards mental health have been undertaken, that finances are not influencing the decision, that there is not undue pressure from family, and so on. These policy issues need to be dealt with, but they do not affect the ethical question of whether there might be any circumstance justifying suicide. If so, then it is a very small moral step to assisted suicide.
Inescapable Pain
When my father was dying of cancer, he was in a terminal coma and receiving as much morphine as the hospice doctor would allow. He was still moaning and writhing in pain. He was certainly both a t’reyfa (someone with an illness that makes death certain) and a goses (someone within days of death), but in truth, that was irrelevant to my thinking. What mattered to me was that he was suffering needlessly and had no hope of returning to meaningful living. Had I had the ability to do so, I would have administered a dose sufficient to alleviate all of his pain. My friend and colleague Elliot Dorff has argued that if pain alleviation is the intention and death only a byproduct, then it is permitted. I would reply that this is a halakhic fig leaf. I would have been grateful to help my father die a few days sooner; only an overly cautious hospice doctor stopped me from doing so. There is no question in my mind but that administering a fatal dose of morphine would have been l’tovato, in his best interest.[fn]See Tosafot, Avoda Zara 27b.[/fn] The quality of palliative care has improved considerably in recent years, but sometimes it is not sufficient. Some doctors quietly make this possible or even secretly administer such a dose themselves.
Many of us know the story of the death of Hanina ben Teradyon.[fn]B. Talmud Avoda Zara 17b-18a.[/fn] Burned at the stake by the Romans, he was suffering greatly when his executioner removed the water-soaked woolen barrier that was meant to make him suffer longer by dying more slowly. For this, Hanina assured the executioner a place in heaven. If Hanina could applaud an act that reduced his suffering in his final hours, then it surely must be ethical to alleviate the suffering of another! The executioner who sped his death is the hero of the story. While this aggadic tale is not a halakhic precedent, it certainly supports the possibility of interpretations about end-of-life pain avoidance.
Loss of Will to Live
I want to share one more kind of story. I knew a Jewish man who was a successful tenured professor. He was well-published and well-liked by his peers, but he suffered from debilitating depression his entire adult life. He had dated occasionally and been in love with several wonderful women, but he could not maintain a long-term relationship because each woman found the depth of his depression overwhelming. He tried literally every known medication and medical treatment, including electroconvulsive therapy, and nothing helped. He gradually told everyone he loved that if nothing changed, he would take his own life because he simply found everyday living too painful. He carefully put all his affairs in order, drove to a parking lot so that he would not make a mess in his home and shot himself. All of us who mourned his loss miss him, but no one I know believes what he did was unjustified. How much better it would have been had there been medication available that would have allowed him to die peacefully at home. Worse yet was the death of another deeply depressed person of my acquaintance who ingested poison and had a horrible death that took several days of agonizing pain, and dragged her family and friends through unspeakable suffering.
When suicide or assisted suicide is being contemplated, it is critical that the decision maker(s) not prematurely give up hope. This is particularly likely to happen in regard to depression, but hope can be prematurely abandoned in the face of a difficult diagnosis as well. Public policy will need to cope with those issues as well.
This essay has argued that there are three clear justifications for suicide, and therefore for assisted suicide: preserving kavod in the face of increasing mental or physical incapacitation; avoiding otherwise inescapable pain; and exhausting the will to live in old age. Given the rapid advances in the field of medicine, I believe it is time for reconsideration of this issue by Jewish bioethicists. Once there is an agreement on even a single ethical circumstance permitting assisted suicide, then we can begin to explore what safeguards would be required to create an acceptable public policy.